Preventing thrombosis by modifying surfaces
Lena Witzdam and Fabian Obstals, scientists at DWI – Leibniz Institute for Interactive Materials works on developing non-thrombogenic surfaces. The focus of their work is to investigate and develop different, so-called "polymer brushes" with hemocompatible properties.
Strokes, heart attacks and pulmonary embolisms are among the most common causes of death in Germany. However, most people are not aware of the fact that their formation in the human body can be favored by using medical products. These include medical devices that are connected to and sometimes implanted inside the patient’s body - such as ventilators (extracorporeal oxygenators, ECMO), cardiac support systems or central catheters. Despite many years of research, it has not been possible yet to avoid such thrombosis complications. The reason is that these medical devices inevitably come into contact with our blood, which can lead to the formation of blood clots (thrombi). These, in turn, can travel along the bloodstream under certain circumstances and for example reach the brain where they trigger a stroke.
In this context, it is important to understand what happens when blood encounters the surface of the medical device: In the human body, the blood normally only has contact with the body's own surfaces like the endothelium. The endothelium is the cell layer on the inside of the blood vessels. In our body, the endothelium has a special task, because it maintains a sensitive balance. This balance fluctuates between activating blood clotting when the vessel walls are damaged to stop bleeding on the one hand and digesting these same blood clots when they are no longer needed on the other. This mechanism responsible for the digestion of the blood clot is called fibrinolysis. In the case of contact with artificial surfaces, such as those of devices for artificial respiration, this interplay does not occur: blood coagulation is inevitably activated by such surfaces, which differ from the endothelium. Thrombi are formed and do not get degraded. If they detach, they can trigger the serious complications described.
In their research project, Lena Witzdam and Fabian Obstals try to find a way to prevent the formation of blood clots on artificial surfaces and even actively control fibrinolysis using surface-modified coatings.
The project - surface modification to prevent and eliminate blood clots
To improve the surfaces of medical devices and products that have contact with blood, Lena Witzdam and Fabian Obstals have taken inspiration from nature. The question at hand: Can the artificial coating of medical devices be designed to mimic the ability of the endothelium? This means that the blood does not directly recognize the coating as "foreign to the body" but, once a blood clot has formed, activate the body's own blood components for its degradation?
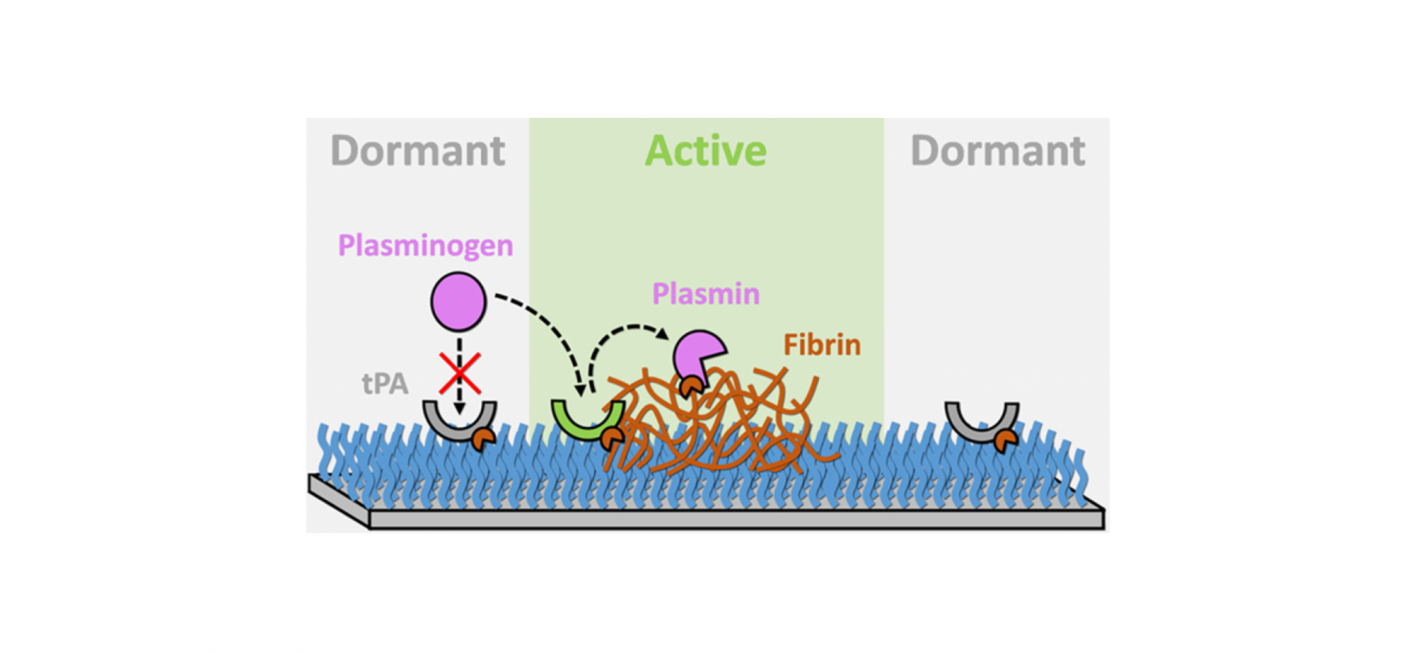
To address this fundamental question, they have developed an ultra-thin coating for biomedical materials. It is made of so-called biofunctionalized polymer brushes and forms the contact surface of the medical device to the blood. The coating can autonomously and reversibly switch between a dormant, non-thrombogenic state and an active, fibrinolytic state when thrombi are present. Therefore, the brushes are equipped with a special enzyme (tissue plasminogen activator, tPA). This enzyme is naturally produced by the endothelial cells of the vessel wall and can enable a localized dissolution of the blood clots (fibrinolysis). This effect is solely and exclusively active when it is required.
This interactive switching between dormant and active states is achieved by a reinforcement mechanism that increases (positive feedback) or restores (negative feedback) the activity of tPA - depending on whether a thrombus is detected and captured or not. Thus, only a low surface density of tPA is required to dissolve thrombi. The research work of Lena Witzdam and Fabian Obstals is the first report on a coating that can self-regulate its fibrinolytic activity depending on the conditions of the blood.
Vision for the future – designing medical products safer for patients
The research team's vision is to create a new generation of hemocompatible surface coatings to make the use of medical devices that interface blood much safer. Their aim is to reduce the risk of thrombotic complications in patients.
Her research, titled "Improving Hemocompatibility: How Can Smart Surfaces Direct Blood To Fight against Thrombi," was published in the ACS Applied Materials & Interfaces Journal.